She’s here! For those of you who haven’t heard, Kaedra Margaret Kaur Rooprai joined us January 9th, after a fast and furious and unexpected labour at 35 weeks plus 4 days. Birth story to come, but suffice to say that birth was as wild, powerful, incredible, and strong as I had thought it would be, and it went as perfectly as I could have imagined with little Kaedra being born in peace at home into mine and her dad’s hands. After a year of being diagnosed with cancer and undergoing cancer treatments while pregnant, birth is one of the easier things I’ve done all year. And that’s not to say it was easy. I said to my doula afterwards “Well – it’s exactly as hard as it looks like it is!”… and exactly as amazing.

Postpartum has been blissful and devastating and calm and emotional. Like my pregnancy, big things to celebrate alongside big things to grieve.
Hours after I posted my last blog update, less than 24 hours after having my drain tube removed which I thought would be the beginning of a break for me until birth, I received a call from my surgeon. She had gotten the pathology report from my surgery, and it wasn’t great. The tissue removed from the breast had responded completely to the chemo, meaning there was no cancer left there at all. However, the lymph area she had removed was not as encouraging. She’s taken out all of the lymph nodes in my left axilla, and all 15 she removed had cancer remaining in them. Most had responded partially to the chemo, but not fully.
I knew right away this was bad news, but I couldn’t bring myself to share it with anyone besides my midwife. I wanted to wait for my oncology appointment to confirm what I suspected and not put bad news onto anyone else sooner than needed and before I had more information.
I’m glad I chose to do that, because I ended up birthing about a week later! I’m so glad bad news from the surgery wasn’t on the forefront of anyone’s mind but mine in those first few magical days postpartum.
And they WERE magical. On a high from our wild birth and meeting out new baby, those first few days were full of the hormones of enamourment. Mom came to town and took care of the cooking and cleaning so Gary could take care of errands and I could take care of Kaedra. I loved breastfeeding her, first with the colostrum I seemed to have plenty of, and then with my milk. I cried when my milk came in – I’d been worried about the chemotherapy impacting my breast development in pregnant and a lot of tissue has been removed from my left breast in the surgery. Both of these made me concerned about the amount of milk I might be able to produce, along with my body just being so stressed during the whole pregnancy. It came in tho and she was so keen for it – what a relief!

As the days went on though, little Kaedra’s started showing signs of a baby not getting enough milk. She was late preterm as well, which can sometimes lead to issues with babies not feeding effectively and combined with my own health picture I started getting worried about her based on her behaviour. She was increasingly fussy at the breast, more and more sleepy, and looking too skinny and a bit jaundice for my eye.
We weighed her with my midwife and my suspicions were confirmed – she had lost much more than the healthy amount of weight and clearly wasn’t getting what she needed from me. The cancer treatments had taken their toll after all.
I felt devastated and guilty and heartbroken. Can’t I get a break and have my body work and have something just go smoothly for more than three days at a time please?!
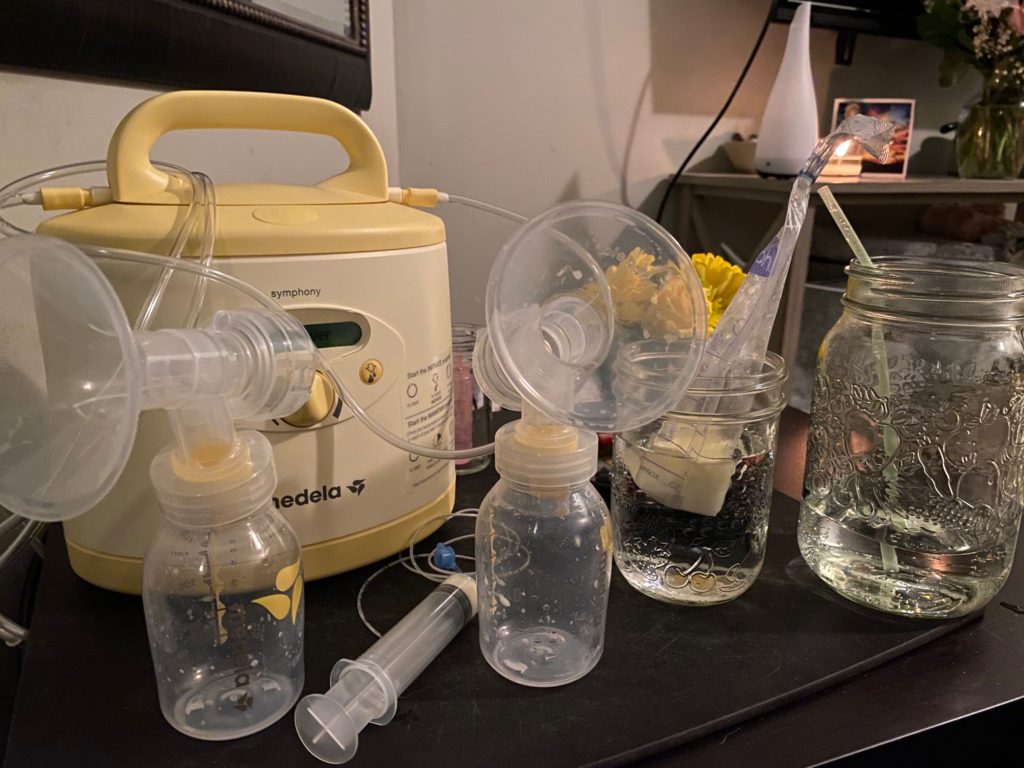
We immediately went into action. My friend Dawn had been pumping for me since my diagnosis, building me a stash in case I needed it. My midwife phoned her and Gary went over to grab frozen milk and tube feeding supplies, making a stop at the herb store for some milk-making herbs. Another friend sent over a breastpump and another a scale, and we got to work.
Plan: Feed the baby. Get my own supply up. Try not to drown in the sadness that I’m not providing nourishment for her from my body the way I so badly want to. There were days of lots and lots and lots of tears and grief – not only that my body was failing Kaedra and I, but inside I also knew I likely had limited time to get my supply up and enjoy breastfeeding her because of the looming oncology appointment and the info I was sure it would bring.

My appointment was scheduled for day 6 postpartum, but I couldn’t bear to bring my 6 day old, pre-term and underweight baby out of the house to have my heart broken further quite yet. I wasn’t ready for my time in my cozy postpartum den to end. I knew delaying my appointment by a handful of days was unlikely to make a big difference to my health cancer wise, but could make a big difference in mine and Kaedra’s health and experience of postpartum. I called my oncologist and he agreed it made sense to shuffle the appointment to the following week.
In the meantime, I was living my life in 3 hour cycles: Breastfeed/Supplement. Pump. Nap. Breastfeed/Supplement. Pump. Nap for 45-60 minutes. Repeat repeat repeat. The only people coming over were my crew of committed midwife friends, checking on us daily to make sure Kaedra and I were doing well – her physically, me emotionally.

She promptly got stronger and more alert every day with our careful routine in the calmness of our home. My emotions were up and down and I don’t want to downplay the grief I felt and still feel about not being able to exclusively feed her. Of course the main thing is her getting fed, and thankfully she was being well nourished with human milk from dear friends as a supplement to what milk I was making for her! But this felt like a huge loss for me in a lot of ways – ways I might detail in another post. I couldn’t help but feel incredibly robbed of a way of caring for her that I was supposed to have the choice to do and value so deeply.
I sent this message to a friend:
I have to admit it’s getting hard to maintain a good relationship with my body at the moment! I feel like I’ve been doing a good job with that so far since diagnosis but having such low milk supply is like pulling out that Jenga piece that leaves the whole thing left feeling wobbly and full of weak points!
Gary was on protector duty for the folks dying to meet and get to know our new little girl. Friends asked to come visit and I told them not yet. Postpartum is such a delicate and sensitive time – so many people full of love for new life and also a fragile hormonal time where the only thing that really matters is the baby being skin to skin on me, eating, learning to feed better at my breast, and me creating the hormonal environment to get my milk supply up along with the technical things I was doing to achieve that as well. Company seems like a small thing, but all too often have I seen the train of visits drain postpartum women, cause too much mother-baby separation, and cause huge issues for their postpartum emotional and physical and their breastfeeding success.
Our culture can be funny when it comes to postpartum, with a lack of understanding of what the mother-baby dyad need for optimal health. People want to come and show their love by “holding the baby”, but it’s really the mother-baby-unit that needs holding: nourishment, calm, peace, to not be separated, to not be kept awake, to not be overstimulated. To just be loved as a unit.
I was okay with people coming by who would crawl into my bed with me while I pumped or breastfed, and who truly understood what I was going through. … People to just sit with us or help us with things like cleaning pumping supplies or bringing me tea or walking my dog, holding then baby only if I needed a minute to go pee, and who would know not to stay too long so that I could focus on being calm and relaxed for the benefit of my hormones. Even then visits distracted me from the feeds that needed all of my focus to go their best as we fought for every ounce, every milliliter of the milk that was perfectly made by my body for hers.
A new mom needs concentration and peace for feeding to go smoothly, and can’t afford to miss her 45min window for a nap in the aforementioned three hour cycle she’s living in! People who spend their time around postpartum women know how important and delicate this time is, and those who don’t have much experience with it don’t, and it’s a delicate balance between bonding to friends and family over meeting the baby in this precious time and disrupting a really important and fragile postpartum window. I always tell my clients: your friends and family have their whole lives to bond to your baby, but you only have one opportunity to set yourself up for a smooth and healthy postpartum and breastfeeding scene!
Read an older post about what a postpartum parent needs here.
Eventually the day came for our oncology appointment, it couldn’t be put off any longer. We packed up our teeny babe (at this point still less than 5lbs!) into the car seat and off we went. Our first outing as a family.
The news came as expected. The pathology meant my prognosis was not great (quite bad actually) and there was a high chance of things spreading, so further chemotherapy was strongly recommended to reduce the risk of that happening. More chemo, a lot of it, and ASAP. And chemo means quitting breastfeeding.
None of this came as a surprise to me, but did confirm my fears and made everything seem more real. It came a bit more as a shock for Gary as I hadn’t had the heart to hammer down his throat the implications of the pathology report before we sat in on this appointment together!
My oncologist also wanted me to go for a PET scan pronto to check whether the cancer had already spread and established itself elsewhere in my body. One was scheduled within a handful of days. The downside to this one? They would inject me with radioactive dye that would be dangerous for Kaedra to be around, so I’d have to be away from her for 6 hours and avoid breastfeeding her for 12 when she was two weeks old.
Not many people leave their two week old babies at all, never mind for 6 hours, and it is just absurd that I had to do so because I’d be RADIOACTIVE. I hated the thought of it so much. I knew she’d be safe and cared for – she’s be with her dad and his sister who I love to pieces would be with him to help. But I shouldn’t have to do this. Most dog breeders say you shouldn’t separate a PUPPY from its mother for 8-12 weeks. There are even laws about it! Tho practically speaking I knew she’d be safe and fed, physiologically, hormonally, biologically speaking it was really not okay that we needed to be separated.
My midwife friend came with me which made the day much easier. We packed Kaedra’s Wonder Woman Cape knitted by my midwife, and my iPhone for music, and a symbolic stone sent by another friend. We packed my breastpump so I could keep pumping while away from her and not compromise my milk production with lack of stimulation more than I had to, even though I would have to throw any milk I pumped down the drain! (I actually almost gave said radioactive milk to her in a moment of brain fog, but that’s another story and I didn’t in the end so all’s well that ends well).
Unbeknownst to me, Amy also had packed a thermos of tea and towels in case I wanted to jump in the ocean to kill some time. She knows me well. After the PET scan, we had lunch and headed down the water for a freezing cold winter dip. This had been a ritual of mine throughout chemotherapy the first time and I’m glad she thought of it – a cold water plunge is always good for the heart and mind and soul!

Finally the 6 hours ended and I was able to go home, back soon to my 3 hour cycle routine. Feed/Supplement, Pump, Nap. Feed/Supplement, Pump, nap. Repeat. For Gary it’s: Feed Jess. Bring her tea. Clean and sterilize pumping supplies. Walk dog. Wash diapers. Run errands. Repeat. Along with a rotating cycle of midwife friends and family members coming round to help me, help him, and bring more milk.
The regimen and our persistence is starting to pay off. My milk is in more every day and she’s having better and better feeds before supplementing, though it’s all a bit feed by feed. It feels good to be working so hard for her/us and even better to have it be paying off, making the most of this short time we have before more chemo.

My PET scan came back mostly clear, with one query spot that will need to be looked at with an MRI. Even if it’s nothing (which my cancer docs think it is), that doesn’t mean there aren’t some rogue unestablished cells floating around, so either way the recommendation remains to do a lot more chemotherapy to kill off those buggers off starting in early February before they get a chance to do any serious harm.
I don’t want to do it. I’m so tired of being a cancer patient. I just want to be a mom. A sleep deprived, leaky breasted, hormonal, breastfeeding mom, worrying about cracked nipples and poopy diapers. I want to be thinking about when our first visit to the forest and ocean together (with her on the outside of my body) will be, not wondering what the long term side effects of chemo might be, and whether or not it will work and be worth it. I want to be thinking about how I can be the best mother I can be to Kaedra, not wondering about how it might impact her if she doesn’t get to keep me.
I feel obligated to do what I can to give myself my best chance of being around for my little family for as long as possible, and afraid of compromising our quality of life too much in our attempts to do that.
That’s not to sound all doom and gloom. A funny thing I’ve noticed about people is they all praise each other for being open and honest and vulnerable but then freak out when anyone says anything too real. We are doing everything we feel makes sense to to take the best care of my health so I can be a mom to Kaedra for a long time. But a little pragmatism is healthy in my opinion.
Our cancer story is unfortunately far from over. Next chemo begins Feb 10th – just four weeks postpartum and only a day after Kaedra’s “due date”. We are plodding ahead, one step at a time, enjoying deeply the moments of just being a new family in the times in between medical appointments and test results and decision making. And we will continue to do so in the months to come, finding the celebration amidst the grief, the dark and the light sight by side just like we have since the early days of getting pregnant and getting diagnosed.
.. I come into the peace of wild things…
This little one takes all my focus and I rarely get (or want) my hands and brain free for long enough to write. But stay tuned for when I post my fun birth story eventually (it was so fun!) and continue to update you now that we are on the postpartum end of this hand we have been dealt together.
My midwife and friend reminded me of some things I often say to clients as encouragement during birth “sometimes I think nature makes it hard as a way to bond us to our babies. When you go through something really challenging with someone, you come out more bonded on the other side.” We sure are getting lots of bonding in, Kaedra. I love you to the moon and back already. These next months and giving up breastfeeding you is going to be really, really hard. And we can do hard things.
